Day in the Life of a Therapeutic Medical Physicist: Nicole Bunda-Randall

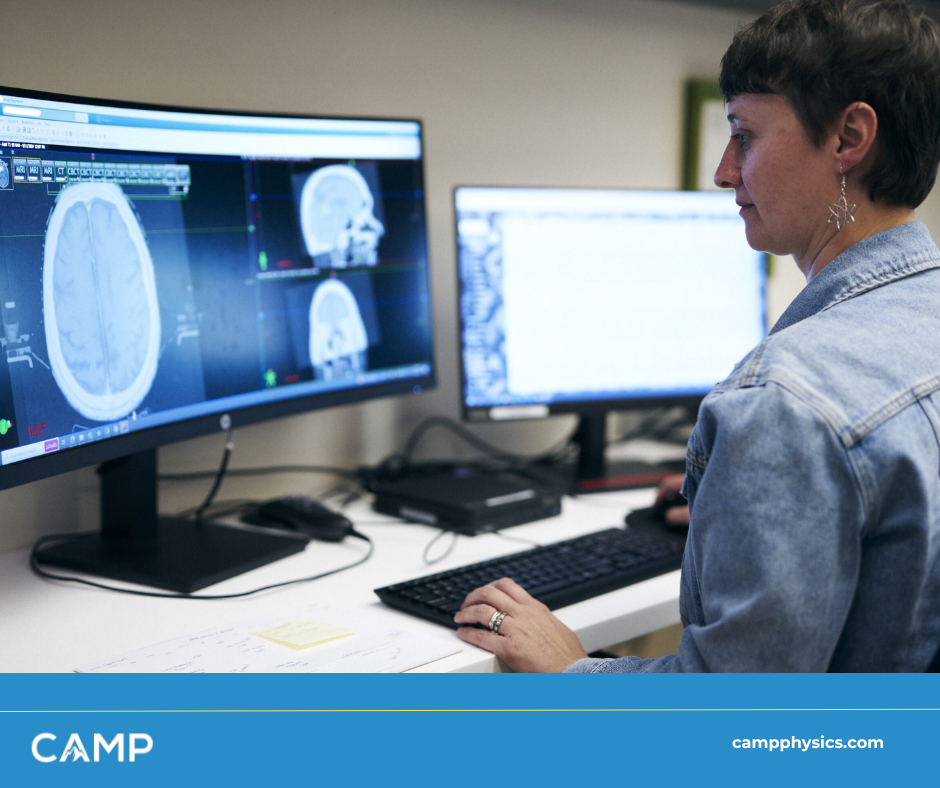
Ever wonder what it’s like to work behind the scenes in radiation oncology, ensuring life-saving treatments are delivered with precision? Therapeutic medical physicists play a crucial role in cancer care, combining science, technology, and teamwork to ensure patient safety and treatment accuracy. We sat down with Nicole Bunda-Randall, a seasoned therapeutic medical physicist at CAMP who regularly provides medical physics support to Parkview Cancer Center, to learn more about her career.
In this interview, Nicole shares the challenges and rewards of her work, explains how medical physics supports cancer patients, and provides insights into what a typical day looks like in one of the busiest radiation oncology departments in the state. From quality assurance (QA) testing on linear accelerators to direct patient interactions during brachytherapy treatments, Nicole’s role is a perfect blend of clinical expertise and problem-solving.
How did you get into medical physics?
I originally wanted to be a lawyer, actually—a patent lawyer. But during undergrad, I got into high-energy research and loved it. Around that time, a friend’s mom, who was undergoing cancer treatment, told me about medical physics. I had no idea the field existed! I was a junior at Purdue, starting to realize that the research path I was on wasn’t for me. When I found out about medical physics, I researched accredited programs and ended up at the University of Kentucky (UK). UK gave me the best offer, and it just clicked. I’ve been working as a therapeutic medical physicist since 2009, and I love it.
What’s your role like in radiation oncology?
I work directly in a cancer center, focusing on radiation oncology. Collaboration is essential in this field. Our team includes physicists, dosimetrists, therapists, doctors, nurses, and administrators. If one part of the team isn’t aligned, things can fall apart quickly.
My main responsibility is quality assurance—daily, monthly, and annual testing of equipment like the linear accelerators, CT simulators, and brachytherapy afterloaders. Every patient who comes in has a treatment plan, and my job is to ensure that the plan is delivered exactly as intended. I also help develop and refine workflows and policies for the clinic, which I really enjoy.
What does a typical day look like for you?
My day starts with equipment checks and QA tests. I’ll warm up the afterloader we use for brachytherapy and make sure the linear accelerators (LINACs) are functioning properly. We also have a morning meeting with the entire department—therapists, doctors, social workers, and dietitians. We go over any new patient starts and address any issues from the previous day.
Throughout the day, I’m troubleshooting equipment or reviewing treatment plans. If the machines throw an error, the therapists call me right away. We also spend a lot of time on image registration, making sure CT, PET, and MRI scans align correctly to deliver the most precise treatment possible.
Do you interact with patients directly?
Most of my patient interaction happens during brachytherapy or CT simulations. During brachytherapy, I’ll walk patients through what to expect—like the sounds they’ll hear and the blinking lights they might see. It’s important to help them feel comfortable, especially since the procedure can be intimidating. While I love being behind the scenes working on processes and QA, I also enjoy these moments with patients. It’s a reminder of why I do what I do!
What excites you most about working in medical physics?
Technology is always evolving, and that keeps me on my toes. For example, we’re now using rapid arc and hyperarc therapies, which allow us to create even more customized treatment plans. The rise of AI and machine learning has also been exciting, especially when it frees us up to focus more on the individual patient.
The most rewarding part is seeing patients thrive. We recently treated a patient with spinal metastases who had already undergone radiation. It was a challenging case, but we came up with a plan that provided relief. Moments like that make it all worth it.
What are the biggest challenges you face in your role?
One of the toughest parts is balancing different personalities within the team. Everyone has the same goal—providing the best care for the patient—but we all come at it from different angles. Developing workflows that meet everyone’s needs can be tricky, but I love that challenge. Keeping up with new research and technology is another big challenge. There’s always something new coming out, and it’s important to stay current while making sure the changes we implement genuinely improve patient care.

What advice would you give to someone interested in medical physics?
Do it! If you love science, math, and problem-solving, it’s a great field. You also need good interpersonal skills because so much of the work involves collaboration. Every day is different, and you have to be ready for anything—whether it’s troubleshooting equipment, developing a treatment plan, or interacting with patients.
What do you find most rewarding about your work?
I love troubleshooting and solving problems. When things go wrong, I enjoy figuring out what happened and how to fix it. I also love writing policies and refining workflows—it’s a bit nerdy, but it’s so satisfying to see processes run smoothly.
The best part, though, is seeing the impact we have on patients. When they come back for follow-ups and their tumors have responded to treatment, it’s the most rewarding feeling. Knowing that I played a part in their care makes everything worthwhile.
How Has Technology Changed Your Work?
AI is great, but I get more excited about how the actual equipment evolves. We’ve seen tools like rapid arc therapy really change the game for patients by customizing treatments in ways we couldn’t before, and now that is advancing further as dynamic rapid arc is being released..
Nicole also noted the growing trend of patients returning for retreatments.
“We’re seeing more patients come back for retreatments, which wasn’t common years ago. Because patients are living longer and thriving, we’ve had to adjust how we approach constraints and planning for retreatments.”
Stereotactic treatments have also been a breakthrough in recent years. For example, linear accelerators are now capable of performing treatments that previously required a Gamma Knife or CyberKnife.
“We’re now able to deliver higher doses in fewer sessions, which helps patients avoid long, difficult commutes for treatment.”
Conclusion
Nicole Bunda-Randall’s career as a therapeutic medical physicist is a blend of science, technology, and teamwork. From running QA tests on cutting-edge equipment to collaborating with colleagues and supporting patients, Nicole’s role is vital to delivering safe and effective radiation therapy. Her passion for problem-solving and her commitment to patient care are clear in everything she does.
“It’s a niche field, but I love it,” she says. “Every day is a new challenge, and I wouldn’t have it any other way.”
Connect with CAMP
Looking to connect with Nicole? Send us a message on LinkedIn.
Want to learn more about health physics, veterinary radiation therapy, and the latest advancements? CAMP offers a wealth of resources and expertise to help you stay informed and engaged in this dynamic field. Whether you’re a healthcare professional, student, or simply curious about the science behind radiation therapy, CAMP is here to support your journey.
Visit our website to explore our services, discover educational opportunities, and join a community dedicated to advancing medical physics.

